News & Updates
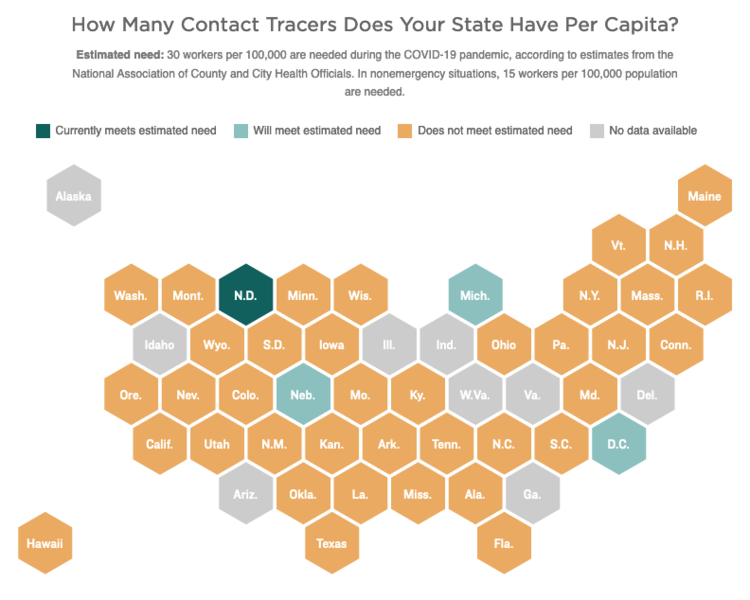
Contact Tracing versus Contact Tracking
Among the many new terms that have crept into our daily language, contact tracing has become one of the most frequently heard in connection with COVID-19. Contact tracing is a traditional public health strategy that has been used to fight the spread of everything from the common flu to the AIDS virus. We often hear public health officials talk about the need to employ contract tracing to not only get the current pandemic under control but to keep the virus from flaring up once we start to reopen cities and states.
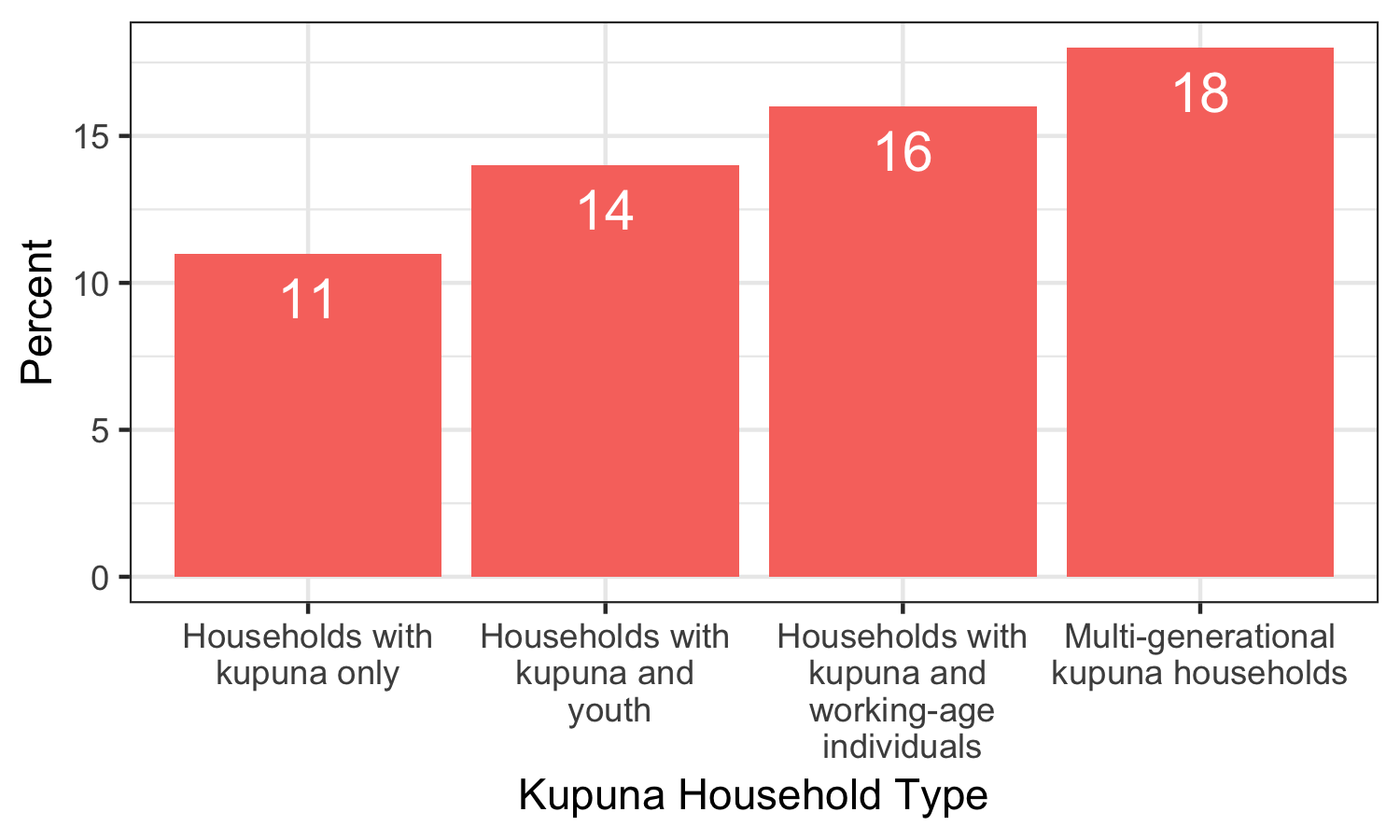
Our Kupuna: Understanding their Risks
Our findings suggest that transmission of COVID-19 is more likely to occur among younger individuals who are more active in the community. In our survey, individuals between the ages of 25 to 44 were the most likely (19%) to report symptoms of COVID-19 or have a household member who tested positive for the virus when compared with other age groups.

Community Vulnerability Index Provides Insights on Pandemic Preparedness
If you’ve done even limited reading about COVID-19 in recent weeks, you’ve likely encountered a short, consistent list of risk factors for individuals developing serious illness from the disease: those ages 65 and older, and anyone with underlying medical conditions. But what do we know about community-level risk for COVID-19? How might we identify which communities are more or less resilient to the current pandemic?
A good place to begin exploring answers to these questions can be found through the COVID-19 Community Vulnerability Index (CCVI).

Ongoing and Comprehensive Information Key to Reopening Hawaii
More importantly, some communities reported higher rates of COVID-19 related symptoms compared to their response rate (e.g. Waianae and Maui)—an indication that these communities may require additional information and resources to mitigate the impacts of the virus. Conversely, communities with lower reported symptoms relative to their response rate may have greater access to information that is helping to protect its citizens (e.g. East Honolulu).

COVID-19 Highlights Vulnerabilities of Rural Hawaii
After an initial delay, cases in rural communities have climbed throughout the country. On March 6, COVID-19 first emerged in Hawaii on its most densely populated island of Oahu. Cases followed in mid-March and early April on the state’s neighbor islands, home to the Hawaii’s more rural areas. As of April 19, 2020, Hawaii Island reported 62 COVID-19 cases; Maui (including Molokai), 106 cases; and Kauai, 21 cases, compared to Oahu’s 385. Although the majority of cases in the state remain on Oahu, the slow and steady growth of confirmed COVID-19 infections on neighbor islands confirms that they are susceptible to the disease as well.
The Good, The Bad, and Social Distancing in Hawaii
During times of crisis, the vulnerable are at even greater risk of becoming casualties of fast moving events. In Hawaii and throughout the nation, we are beginning to see how the current pandemic is overwhelming seniors, those living in poverty, those living on the edge of poverty, and the homeless. They are the most vulnerable in these times. And while they may be overwhelmed, in Hawaii, they are never left behind. That is not what we do nor who we are.
Local Expert-Driven COVID-19 Models for Hawaii Are Long Overdue
We learned the hard way that modeling COVID-19 forecasts is not one-size-fits-all. Recently, we wrote about the advantages of the University of Washington IHME model for understanding peak hospital demand in Hawaii, only to shortly thereafter advise caution in interpreting the model because the projected hospital capacity peak had suddenly shifted by three weeks [link]. A closer inspection of the model revealed problematic assumptions, and underscored a real vulnerability for Hawaii in not having a valid local model.

Insights from the Hawaii COVID Contact Tracking Survey
This is the first in a series posts highlighting results from the Hawaii COVID Contact Tracking Survey conducted by the National Disaster Preparedness Training Center (NDPTC) and the Pacific Urban Resilience Lab (PURL) at University of Hawaii at Manoa. The Hawaii Data Collaborative has partnered with this group to share regular analyses and updates from this survey in the coming weeks.
[Updated] Can Hawaii's Hospitals Meet Peak COVID-19 Demand?
We have been working to evaluate multiple modeling tools for projecting peak hospital demand and capacity sufficiency in Hawaii. The University of Washington (UW) Institute for Health Metrics and Evaluation (IHME) model was identified as best suited for projecting Hawaii hospital capacity in the coming weeks.
Understanding COVID-19 Transmission in Hawaii
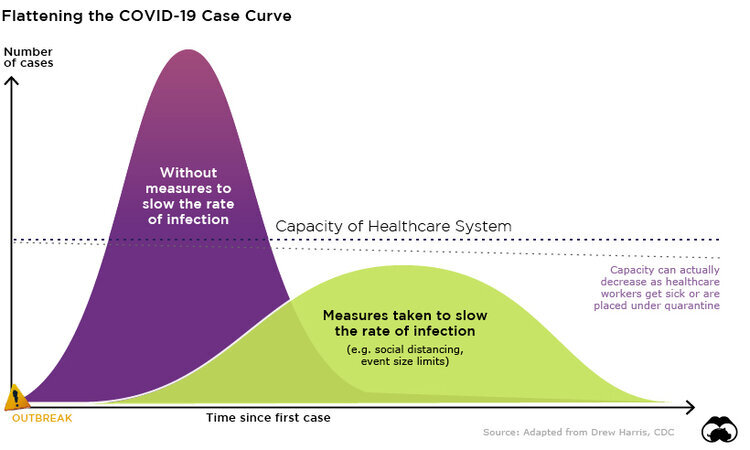
To help illustrate the role of social distancing measures in preventing the spread of COVID-19, we have been working to adapt current transmission models for Hawaii… you can see how existing mitigation efforts are projected to influence the spread of the virus, as compared to no action and more aggressive measures… These forecasts were generated using an accessible modeling tool created by researchers at the University of Basel in Switzerland. This model is updated continuously as new information about COVID-19 becomes available.

Hawaii Financial Health Pulse Report Provides In-Depth View of Residents' Financial Struggles
A study released yesterday further substantiates the financial hardships faced by, and resilience exhibited by, people living in Hawaii. The Hawaii Financial Health Pulse, sponsored by Hawaii Community Foundation and Bank of Hawaii, is a localized version of the U.S. Financial Health Pulse, which examines the financial health of Americans. In close collaboration with local advisors, The Financial Health Network surveyed more than 1,600 Hawaii residents to better understand their “financial health”—that is, how they spend, save, borrow, and plan in their financial lives.

Newly Released CDC Estimates Reveal Community-Level Health Indicators
Recently the 500 Cities project, a collaboration between the U.S. Centers for Disease Control and Prevention (CDC) and the Robert Wood Johnson Foundation, released small-area estimates of health outcomes, risk factors, and healthcare usage for the 500 largest cities in the U.S. While health measures are often reported at the state level, the 500 Cities project seeks to equip local health stakeholders with more granular estimates of community health data, thereby informing important policy, planning, and programmatic decision-making.